Introduction
In 2020, I wrote a blog titled From Telegraph Road to US$50 Billion Digital Health Silk Road Digital Health Silk Road Archives | Kapil Khandelwal KK celebrating the announcement of the National Digital Health Mission (NDHM) under the National Health Authority (NHA). We had worked out the direct and indirect impaction to the Indian economy that such an initiative will result. Over the next few years, the turn of events have led the country to not move forward on such a huge initiative for the healthcare of people of India. Let’s look at the turn of events leading up to the recent development and the way forward from here.
Key Developments in the Journey of Developing our Universal Health Initiative (UHI)
‘National Health Stack – Strategy and Approach’
In 2018, NITI Aayog released a document setting out the building blocks of the National Health Stack as ‘common public goods’ which are essential for an implementation of digital health initiatives in India. The key components described in the National Health Stack were national health electronic registries, claims platform, federated personal health records framework, national health analytics platform, and other horizontal components.
National Digital Health Blueprint (NDHB).
In 2019, Ministry of Health and Family Welfare (MoHFW) released the National Digital Health Blueprint (NDHB). The need for creating a framework for the evolution of a ‘National Digital Health Ecosystem’ (NDHE) – an ecosystem and not a system, was recognized in the NDHB. The NDHB lists out principles, building blocks, applications and digital services, standards, institutional frameworks etc, to create such an ecosystem.
National Telemedicine Guidelines
During Covid, the Medical Council of India (MCI) quickly released the National Telemedicine Guildlines to enable tele consultations so that limited capacity of the physicians is utilised for remote consultations during the pandemic and lockdowns.
Consultation Paper on Unified Health Interface (UHI)
In March 2021, MoHFW released a consultation paper on Unified Health Interface (UHI) to replicate its digital-payment success in healthcare. Taking cues from the Unified Payments Interface (UPI), it set out to establish a similar system for healthcare inclusion and universal health for the people on a ‘Bharat Stack’ for Healthcare. I am sure many of the tech industry bodies such as Nasscom, iSpirit and CII and FICCI would also have been consulted in framing the Consultation Paper.
Current Status
iSpirit, Indian tech industry body was appointed by National Health Authority (NHA) to lead the development of UHI. There have been delays in operationalizing the UHI and recent media reports state that key disagreement between the NHA and iSpirt on the nature of the UHI network-and iSpirit walking away from the project.
Why Did UHI not take Off?
iSpirit and Media View Points
There is a long format article from Ken that has been doing rounds and my talks with some of the Healthtech and other VC investors interested in this initiative have been summarized here:
- Limited use of iSpirit partners for building components
- Rationale of iSpirit partners that were short-listed for pilot and those left out for the wider roll out in the next stage
- Conflict of interest between the iSpirit partners shortlisted that would push their product/components into the UHI pilot making it not a fully open system
- Lack of openness between the iSpirit and NHA on the development and roadmap for wider participation of healthcare industry players
- Slippage of deadlines for the teleconsultation solution multiple times drawing the ire of NHA
- Self-doubts within iSpirit on the future success of the pilot and the eventual scale of UHI
- iSpirits experience with other non-healthcare solutions roll-outs on the way forward in the roll out of UHI to the nation which is not true for healthcare as compared to fintech, social commerce and other digital solutions
My Views on Current UHI’s State
Let me tackle the lack of understanding of the reality of the Indian healthcare system and how it is evolving in the future for the UHI to succeed. These are some of the points that I have made in the past in various industry forum presentations, my articles and blogs. Then I will address the way forward from here for UHI to succeed
India’s Scale in UHI will be an Aggregation of its Diversity of People – The Markers for Healthcare Delivery
Based on my experience of rolling out the 104 and 108 helplines in late 2000s, for any solution to be successful, especially the teleconsultation that iSpirit and NHA were developing, it has to build for the different languages and dialects prevalent not only in a region of a state, but across states due to floating population. As recently as covid pandemic, when we were rolling out CovidBots for triage on the 104 for a few states, we have realized that nothing has changed in the last 20 years in India. The figure below provides the language diversity for which we will need to implement not a one product fits all under UHI.

With the best of the cloud services, India has a limitation of 23 languages being provided with voice translation capabilities.
What Scale are we talking of?
Based on our population genetic, epidemiological, chronic disease burden, I had released this state-wise risk map of India in 2010. This show that we have around 50 million households which have high-risk burden. This is twice as big as the population of USA. This is expected to touch over USD 150 bn of spend not just on curative but preventive care.

So what is the scale we are talking of? Is this not sizeable according to iSpirit? How does this compare with the subscribers are using UPI? As of July 2021, there were around 130 million monthly active subscribers on UPI after 5 years of its launch. As per industry estimates if I recall, the digital health services teleconsultations peaked during Covid lockdown and were around 100 million monthly active subscribers/teleconsultations consultations. This is even before the launch of teleconsultations module of UHI. Can you imagine the multiplier effect once it goes mainstream?
Why Not Partner with Nasscom’s Tech Services Companies?
On the issue of openness between iSpirit and NHA on the development and roadmap for wider participation of healthcare industry players, my take is that iSpirit’s objective is to promote product players from India. But, I must remind that large IT services players like Wipro, Infosys, Cognizant, TCS, IBM, Tech Mahindra, etc who have been building point-solutions for some of the leading healthcare players and governments globally for over twenty years. Not inviting and leveraging these partners from Nasscom is also one of the reasons for failure of UHI
Learning from Past Mega Global Healthtech Product Failures
I have written in the past on why global players with deep pockets like Google, Microsoft, IBM, etc have failed on their healthcare initiatives. National Digital Health Archives | Kapil Khandelwal KK Haven’t we any learnings from such mega failures?

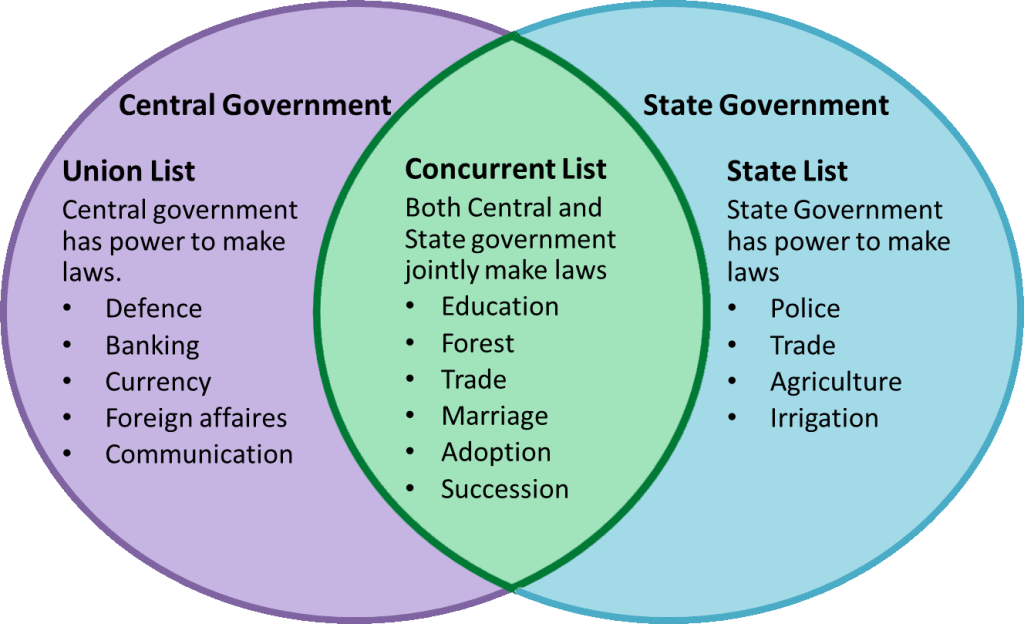
Digital Health Penetration Across States is Not Uniform Nor is State-wise Regulations
In our 2021, State Healthcare Heat Map 2021 States Heat Map | Kapil Khandelwal KK, the first of its kind report for which are the hottest states to invest in healthcare, we have covered factors like Penetration of Digital Health. It is very clear that UHI to be successful, it is not going piecemeal staggered solutions go-live, but a big-bang all UHI solutions go-live in the states with highest digital health penetration. Moreover, have we not learnt lessons on how each of the states managed the delivery of Covid Care Sustainability Of Digital Health | Kapil Khandelwal KK as healthcare is a state subject. Have we not forgotten that West Bengal is not there for running the Ayushman Bharat. Nor does it run the National Health Emergency Ambulance number 108. Assuming, even if UHI would have gone live, there would be another layer of customisation that UHI would have to roll out for each of the states where the healthcare is delivered. Different states are at different maturity of implementation of various medical criminal code and consumer protection. Such state regulations and code cannot be circumvented by one EULA of the UHI and the modules. We are not transferring money like UPI, we are managing health of the people where there are risks of lives.

Start with the Building Blocks
Post Covid, a lot has changed. Since UHI wanted to start with teleconsultations, can we even get the ICD-11 codes live in India so that we are up to international standards? Since outpatient consultations/teleconsultations are predominantly out of pocket spend, there is least incentive for the care giver on the street to fill up the forms and ICD codes. With ICD coding in the UHI, AI tools at the back end would be able to assist not only the care givers but also the consumers, the other ancillary benefits of coding would follow.
In Conclusion
Setting aside the differences, it is clear that UHI’s scale and opportunity is even bigger than UPI’s and its impact on the people of India once it is fully implemented and evangalised by each of the states of India. Comparing success of UPI to UHI will be a totally wrong starting point. UHI is like the GST (GST has its own set of issues) with each state having its say in the GST Counsil. Let us reenergize the UHI with bringing in the States and Nasscom players into the solution to make it more viable and successful.